When Obamacare (ACA) hit the insurance market in 2010, it caused major waves for carriers, policyholders, agents, and health care providers. With expanded plans required to cover a minimum of ten essential benefits, the ACA made it so that more people had access to preventative and beneficial health coverage, regardless of income. One of the larger shifts was the mandatory coverage of mental health services through the ACA.
Mental Health Services Through the ACA
As listed on HealthCare.gov, one of the ten essential benefits ACA plans must cover is “mental health and substance use disorder services, including behavioral health treatment,” along with counseling and psychotherapy. The law also protects those with a history of mental illness or substance abuse by requiring all private insurance companies to cover those with pre-existing conditions.
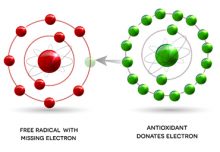
Before the ACA went into effect, insurance providers rarely provided any coverage for mental health disorders. Experts like Senior Vice President of Public Policy & Advocacy Heather O’Donnell of Thresholds, a Chicago-based treatment provider that helps those with mental health and substance abuse issues, largely attribute this to the dark history of mental illness treatments and the stigma that still surrounds mental health today.
Past Mental Health Services
The offered mental health services through the ACA affect both the private and public insurance markets, including both individual plans and Medicaid coverage. Medicaid helps provide lower-income individuals and families cover the cost of health care services. By expanding services, the ACA allowed more people with significant mental illnesses access to coverage throughout the past decade.
Researchers in a 2015 study for the Centers for Disease Control and Prevention found that those with serious psychological distress were between seven and 17 times more likely to be on public insurance plans, like Medicaid, than private insurance plans between 2012 and 2015. Researchers defined serious psychological distress as experiencing mental health conditions to a severe enough extent that the conditions affected school, work, or social behavior. Among this same group, however, the number of people with private insurance plans rose over 8 percent during the study while the number of those with public health plans remained the same.
Moving Forward
The ACA’s mental health measures expanded the reach of the 2008 mental health parity law, which ruled that insurers must treat mental illnesses like they do other types of illnesses. Though the act has drastically improved the dynamic between insurance companies and patients with mental illness or facing substance abuse, America has a long way to go in ensuring mental health and physical health are viewed with the same sense of severity and urgency. The first step in resolving the remaining issues is to dissolve the overarching stigma that surrounds mental health.
Agents
We hope this information on mental health services through the ACA is helpful to you.
Empower Brokerage is dedicated to helping you educate your clients on the insurance they need and staying on top of their health. Whether it’s through webinar training, one-on-one calls, seminars, or marketing plans. We want you to be successful. Give us a call if you have any questions at 888-539-1633.
Quick Links:
• Get Customized Marketing Materials
Originally from the snow-capped Rockies, Macee moved to Texas in 2016 to pursue an undergraduate degree in Strategic Communication. She currently serves as a writer and editor for Empower Brokerage, as well as the marketing manager for Preferred Senior Advisors. Macee is also working on her Master’s degree in management, and hopes to inspire others with her passion for telling stories through varied digital and print marketing efforts.